Main navigation

Research
Key to the College’s strong research culture was the creation of an Office of Nursing Research in 1984 under the direction of Dr. Toni Tripp-Reimer. This office became an official partnership with UIHC in 1989, and fostered research collaborations while also providing support for identifying funding opportunities, developing research grant applications, managing and analyzing data, and manuscript preparation.
As the college built its research base, multiple areas of strength emerged. Dr. Connie Delaney (78MA) began and led the informatics program in the 80s and 90s, and Drs. Janet Williams (68BSN, 72MA) and Sandra Daack-Hirsch (86BSN, 98MSN, 07PhD) led pioneering research in genomics. Drs. Toni Tripp Reimer, Kathleen “Kitty” Buckwalter (71BSN, 76MA), Keela Herr, Meridean Maas (57BSN, 60MA), and Janet Specht (73BSN, 81MA, 96PhD) blazed a path in gerontology and gerontological pain. Dr. M. Kathleen Clark conducted research on women’s health and Drs. Ada Jacox, Joann Eland (70BSN, 74MA), Ann Marie McCarthy, and Charmaine Kleiber (99PhD) produced impactful research and tools to assess and address pediatric pain. Dr. Rita Frantz (73MA) led research on wound healing that influenced Dr. Sue Gardner’s (81BSN, 90MA, 99PhD) research on wound care and Dr. Barbara Rakel’s (79BSN, 88MA, 02PhD) investigations of non-pharmacological strategies to reduce movement evoked pain. Influential in the field of nursing administration were Drs. Myrtle Kitchell Aydelotte, Mary Blegen (75MA), Meridean Maas, and Marita Titler (78MA, 92PhD), while Drs. Gloria Bulechek (63BSN, 67MA) and Joanne McCloskey were instrumental to the creation of a taxonomy of nursing intervention and outcomes.
College of Nursing research has often been cited throughout the years, and early research continues to be held as a standard when developing new practices and policies in care settings. A few of the most cited works by Iowa Nursing faculty include:
Blegen M.A. (1993). Nurses’ job satisfaction: A meta-analysis of related variables. Nursing Research, 42(1) 36-41.
Mueller C.W., McCloskey J.C. (1990). Nurses’ job satisfaction: A proposed measure. Nursing Research, 39(2) 113-117.
Since 2004 there have been 560 requests for the Mueller McCloskey Job Satisfaction Scale.
Butcher H.K., Holkup P.A., Buckwalter K.C. (2001). The experience of caring for a family member with Alzheimer’s disease. Western Journal of Nursing Research, 23(1) 33-55.
Maas M.L., Reed D., Park M., Specht J.P., Schutte D., Kelley L.S., Swanson E.A., Tripp-Reimer T., Buckwalter K.C. (2004). Outcomes of family involvement in care intervention for caregivers of individuals with dementia. Nursing Research, 53(2) 76-86.
Herr K., Coyne P.J., Key T., Manworren R., McCaffery M., Merkel S., Pelosi-Kelly J., Wild L. (2006). Pain Assessment in the Nonverbal Patient: Position Statement with Clinical Practice Recommendations. Pain Management Nursing, 7(2) 44-52.
Kleiber C., Harper D.C. (1999). Effects of distraction on children’s pain and distress during medical procedures: A meta-analysis. Nursing Research, 48(1) 44-49.
Hanrahan K., McCarthy A.M., Kleiber C., Lutgendorf S., Tsalikian E. (2006). Strategies for salivary cortisol collection and analysis in research with children. Applied Nursing Research, 19(2) 95-101.
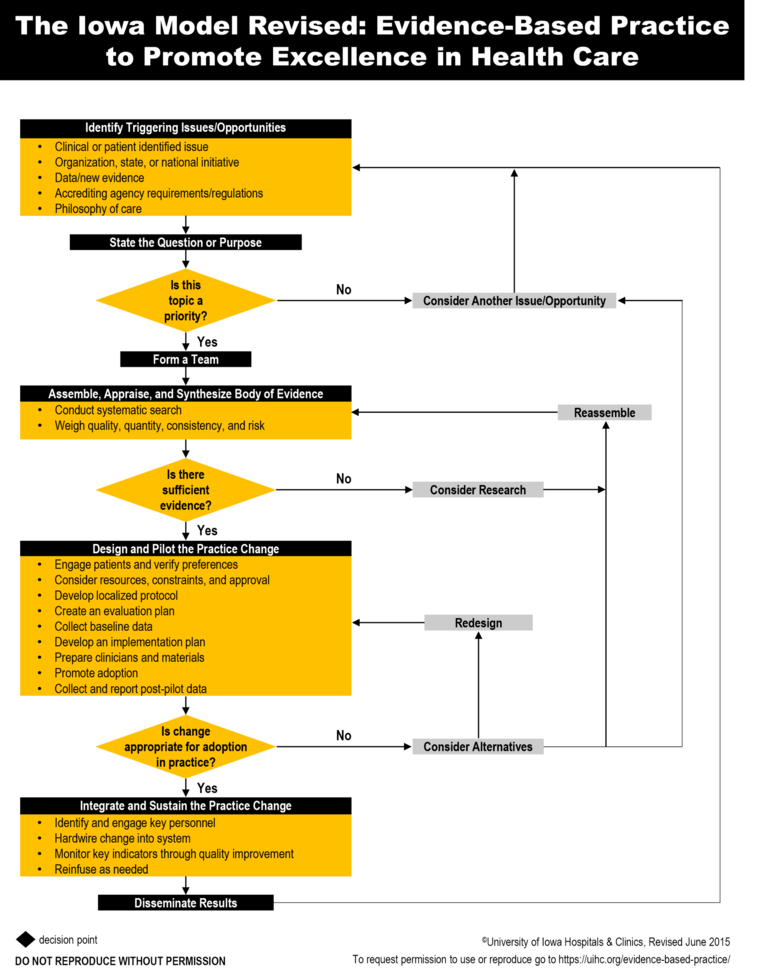
Titler M.G., Kleiber C., Steelman V.J., Rakel B.A., Budreau G., Everett L.Q., Buckwalter K.C., Tripp-Reimer T., Goode C.J. (2001). The Iowa Model of Evidence-Based Practice to Promote Quality Care. Critical care nursing clinics of North America, 13(4) 497-509.
Iowa Model Collaborative, Buckwalter K.C., Cullen L., Hanrahan K., Kleiber C., McCarthy A.M., Rakel B., Steelman V., Tripp-Reimer T., Tucker S. (2017). Iowa Model of Evidence-Based Practice: Revisions and Validation. Worldviews on Evidence-Based Nursing, 14(3) 175-182.
Holkup P.A., Tripp-Reimer T., Salois E.M., Weinert C. (2004). Community-based participatory research: An approach to intervention research with a Native American community. Advances in Nursing Science, 27(3) 162-175.
The language of nursing care

The Center for Nursing Classification and Clinical Effectiveness, an Iowa Board of Regents-approved Center, was established in 1995 to facilitate the ongoing research and development of the comprehensive, research-based, standardized classifications commonly known as NIC (Nursing Interventions Classification) and NOC (Nursing Outcomes Classification).
These classifications provide a set of terms to describe nursing treatments and nursing-sensitive patient outcomes and, in conjunction with North American Nursing Diagnosis Association-International (NANDA-I) diagnoses, serve as the foundation for nursing process in nursing practice, education, and research.
For example, NANDA-I is used to diagnose a person’s health problems, NOC to set desirable outcomes for the diagnosis, and NIC to provide the interventions to achieve the NOC outcomes.
Collectively, NIC, NOC, and NANDA-I, often referred to as NNN, are used in 28 countries.
“My vision is that NIC and NOC classification, in partnership with NANDA-I, are used to improve human health. To do this, it is imperative that we demonstrate the value of nursing classifications. This will require both expanded use in practice and innovative use with patients that demonstrates the value of nursing care.”
–Karen Dunn Lopez (08PhD), CNC director, 2020–present
12,266
Iowa Model requests/downloads from 50 states and 68 countries; cited 1,526 times
*as of Aug. 7, 2023
The Iowa Model and Evidence Based Practice

31,227
Requests/downloads of "Evidence Based Practice in Action", from 53 countries, 50 states, and cited 119 times
*as of Aug. 7, 2023